"Patients who do not share a bedroom
and have generalized tonic-clonic seizures
had 67 times the risk of SUDEP."14
Even a brief discussion with patients and their caregivers
about SUDEP may save lives.3

"Patients with breakthrough seizures
had 8.1 times higher epilepsy-related
financial costs."14
Help your patients Manage the risks
and Avoid the costs.
Use the Breakthrough Seizure Risk Assessment
Tool as a starting point to discuss your patient's risk
factors for breakthrough seizures.
"I'm facing significant life events
(such as changes to relationships,
moving, a new job)."
HCP RISK ASSESSMENT TOOL
PATIENT RISK ASSESSMENT TOOL
Use the Breakthrough Seizure Risk Assessment
Tool as a starting point to discuss your patient's risk
factors for breakthrough seizures.
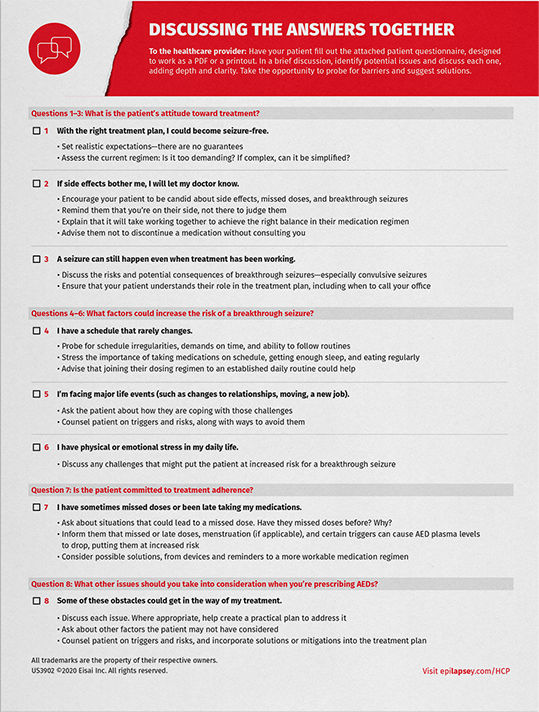
"What is the patient's attitude
toward treatment?"
HCP RISK ASSESSMENT TOOL
PATIENT RISK ASSESSMENT TOOL
BREAKTHROUGH SEIZURE RISK
ASSESSMENT TOOL
Use this tool with your patients as a quick way to learn
which risk factors for breakthrough seizures are most
prevalent in their lives.
PATIENT RISK ASSESSMENT TOOL


SUDEP DISCUSSION GUIDE
Even a brief discussion with patients and their
caregivers about SUDEP may save lives.3
SUDEP=sudden unexpected death in epilepsy

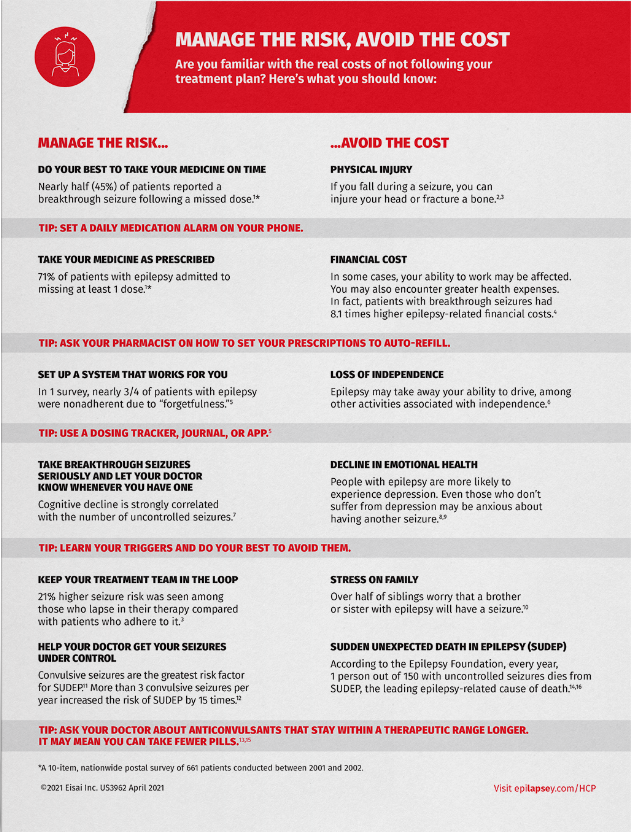
MANAGE THE RISK,
AVOID THE COST
What are the costs of not managing the risk of
breakthrough seizures? Have these talking points
at hand to share with patients.
Talk with your patients about breakthrough seizures—
especially convulsive seizures.
Some anticonvulsants have a narrow therapeutic range.29 Discuss a treatment
option that may help mitigate some of the risk.